Knee joint
Knee joint: function, injuries and treatment options
Sports injuries to the knee joint can result from both accidents (traumatic) and sustained overuse (chronic). Traumatic injuries usually affect the ligaments (e.g., cruciate ligament tear) and the menisci (e.g., meniscus tear). Chronic damage primarily affects the cartilage, which can become thinned due to sustained overuse (beginning of joint wear = osteoarthritis).
Our department specializes in the treatment of ligament tears, meniscus injuries, cartilage damage, joint wear (osteoarthritis), and leg misalignments. We also treat all injuries related to the kneecap.
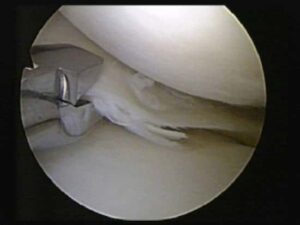
Many of the knee surgeries performed in our department are performed arthroscopically. This involves only small incisions (known as the keyhole technique), and a camera is inserted into the knee joint.
Arthroscopy of the knee joint.

Arthroscopy of the knee joint. The left image shows a camera being inserted into the knee joint. The right image shows an arthroscopic image as seen on monitors in the operating room.
Ligament tears: causes and treatment
The primary function of ligaments is to stabilize the knee joint. A tear in one or more ligaments therefore leads to an unstable knee joint, which prevents the patient from participating in sports. In the long term, an unstable knee joint also leads to incorrect loading of the cartilage and meniscus, which can cause damage to these structures.
Anterior cruciate ligament (ACL)
A clever anterior cruciate ligament It usually does not heal, so replacement of this ligament is usually recommended for active patients. To replace the anterior cruciate ligament, our department prefers knee flexor tendons (the tendons of the semitendinosus and gracilis muscles) (Fig. 2), which are inserted into the knee joint via drilled channels in the upper and lower leg (Fig. 3).

Fig. 2: Tendon grafts prepared for anterior cruciate ligament replacement (autologous knee flexor tendons).

Fig. 3: Left image: Intact anterior cruciate ligament; Middle image: torn anterior cruciate ligament; Right image: Anterior cruciate ligament replaced with autologous hamstring tendons.
Posterior cruciate ligament (PCL)
A posterior cruciate ligament tear can often be treated early on without surgery. Special splints, worn for at least 12 weeks, attempt to bring the ligament ends together so they can heal. For tears that occurred earlier or for insufficient stability after splinting, the ligament is replaced arthroscopically with the body's own tendons, similar to the anterior cruciate ligament.

Fig. 4: Left image: Intact posterior cruciate ligament; right image: Posterior cruciate ligament replaced with autologous knee flexor tendons.
collateral ligaments
- Inner band: Surgery is often not necessary; the tear usually heals by wearing a splint for 6 weeks.
- Outer band: However, surgery is often required. Depending on the location and severity of the tear, the ligament is sutured, fixed to the thigh or lower leg using small bone anchors, or replaced with a tendon from the body.
Complex ligament injuries

Lateral ligament replaced with a tendon from the body.

Meniscus injuries: causes and treatment
Function of the menisci:
The two menisci (median and lateral meniscus) play an important role in load transfer within the knee joint. If meniscal tissue is lost, pressure on the cartilage increases, causing long-term damage and potentially leading to osteoarthritis (joint wear). Meniscus tears usually become noticeable through pain during exertion (e.g. twisting movements).
Treatment options
- Meniscus suture: In suitable tears, especially in the well-vascularized area of the meniscus, sutures are used to preserve the tissue.

- Partial resection: If suturing is not possible, only the damaged parts of the meniscus are removed to preserve as much functional tissue as possible.
Meniscus replacement
If a large part of the meniscus had to be removed in a previous operation, in certain cases the implantation of a replacement meniscus can be considered for long-term protection of the articular cartilage, especially in young patients.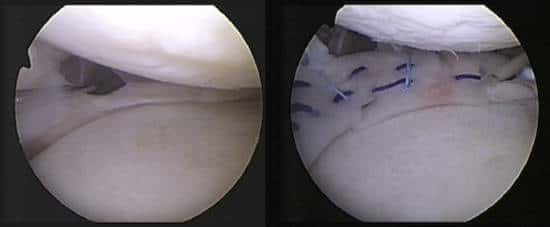
Left image: Meniscus present only in the peripheral area; Right image: Knee joint after implantation of a replacement meniscus made of collagen.
Individual advice & state-of-the-art treatment methods
Minimally invasive & innovative surgical techniques
Quick return to everyday life, work & sport
Cartilage damage: causes and treatment
Causes
Treatment options
- Microfracture: Drilling into the bone beneath the cartilage damage to promote the formation of replacement cartilage.
- Cartilage transplantation: Transplantation of the body's own cartilage tissue into the damaged area.
- Cartilage-bone cylinder transplantation (OATS): Transfer of cartilage-bone cylinders from less stressed areas into the defect.

Osteoarthritis (joint wear): causes and treatment
Causes
Treatment options
- Conservative: Physiotherapy, pain medication and injections.
- Operational: In advanced cases of osteoarthritis, joint replacement (endoprosthesis) may be necessary to improve function and quality of life.

Fig. 9: Loading of the knee joint in a bow-legged patient. The red line describes the loading axis, which runs from the femoral head to the ankle joint. In a bow-legged patient, this line intersects the knee joint in the inner part of the knee joint.
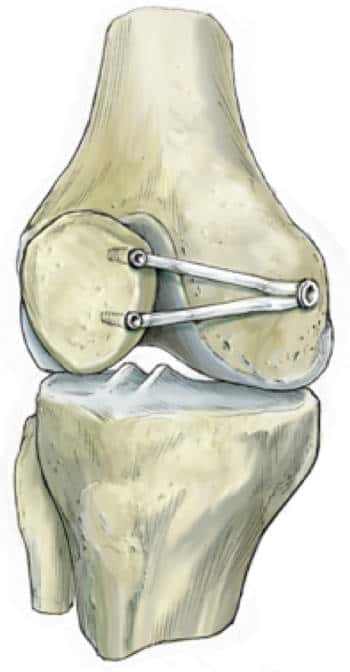
Leg misalignments and realignment operations
With bowlegs, the load axis runs through the inner part of the knee joint (Fig. 9). Over time, this can lead to excessive strain, pain, and cartilage wear (osteoarthritis). With knock-knees, the outer part of the knee joint is correspondingly overloaded.
Conversion operation
In cases of misalignment, a so-called realignment surgery can be performed. This involves a saw cut in the bone to correct the alignment of the leg, thus relieving pressure on the damaged part of the joint.

Left image: The red line shows the load axis before the saw cut. This runs through the inner part of the knee joint. Right image: The green line shows the load axis after the saw cut and subsequent correction of the leg axis. The load now runs significantly further outward, thus relieving the damaged inner part of the joint.
Depending on whether the deformity originates in the upper or lower leg, the saw cut is also made on the lower or thigh. For bowlegs, the correction is usually made on the lower leg, while for knock-knees, it is usually made on the thigh.
After the correction, the bone must first be stabilized with a plate, as with a bone fracture, which can be removed after about one year.

X-ray image after a lower leg realignment surgery for a bowleg. The saw cut was stabilized with a carbon compound plate.
Injuries to the kneecap
Patellar luxation and surgical stabilization
After a dislocation of the kneecap (so-called patellar luxation), the kneecap usually becomes unstable, with it repeatedly "popping out." In addition to significantly limiting the patient's ability to participate in sports or everyday activities, this also leads to increasing cartilage damage. Surgical stabilization of the kneecap is therefore recommended, especially in younger patients. The most common surgical procedure involves replacing the patella's supporting ligament (the medial patellofemoral ligament) with an autologous tendon (the gracilis muscle tendon) (Fig. 12).
Risk factors for patellar instability
Treatment of cartilage damage of the kneecap
Cartilage damage to the kneecap is treated in the same way as other cartilage damage. Further information on the treatment of Cartilage damage.
Mini prosthesis for advanced osteoarthritis
Our department has particular experience in partial kneecap replacement. This becomes necessary when the joint cartilage is already at an advanced stage of wear and tear and biological procedures, such as cartilage cell transplantation, are no longer feasible. In this case, the damaged area is replaced with a special mini-prosthesis, which was co-developed by our department.

X-rays after partial kneecap replacement with a mini prosthesis.
Make an appointment now!
Are you suffering from knee pain or an injury? Our specialists at Munich Sports Orthopedics offer state-of-the-art diagnostics and customized treatments.
Get advice!
Make an appointment now for a personal examination and treatment:
+49-(0)89 4140-7840
sportortho@mri.tum.de
House 524
Ismaninger Str. 22
81675 Munich

