Kniegelenk
Kniegelenk: Funktion, Verletzungen und Behandlungsmöglichkeiten
Sportverletzungen am Kniegelenk können sowohl durch Unfälle (traumatisch) als auch durch andauernde Überlastung (chronisch) entstehen. Traumatische Verletzungen betreffen in der Regel die Bänder (z.B. Kreuzbandriss) und die Menisken (z.B. Meniskusriss). Chronische Schädigungen betreffen vor allem den Knorpel, der durch andauernde Überlastung ausgedünnt sein kann (beginnender Gelenkverschleiß = Arthrose).
Unsere Abteilung spezialisiert sich auf die Behandlung von Bänderrissen, Meniskusverletzungen, Knorpelschäden, Gelenkverschleiß (Arthrose) und Fehlstellungen der Beine. Zudem behandeln wir sämtliche Verletzungen rund um die Kniescheibe.
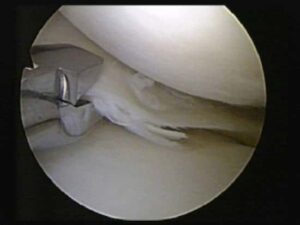
Viele der in unserer Abteilung angebotenen Knieoperationen werden arthroskopisch durchgeführt. Hierbei werden nur kleine Schnitte benötigt (sogenannte Schlüsselloch-Technik), und eine Kamera wird ins Kniegelenk eingeführt.
Arthroskopie des Kniegelenks.

Arthroskopie des Kniegelenks. Auf dem linken Bild ist zu sehen wie eine Kamera ins Kniegelenk eingebracht wird. Das rechte Bild zeigt eine arthroskopische Aufnahme wie sie auf Monitoren im OP-Saal zu sehen ist.
Bänderrisse: Ursachen und Behandlung
Die Hauptfunktion von Bändern ist die Stabilisierung des Kniegelenkes. Ein Riss eines oder mehrerer Bänder führt daher zu einem instabilen Kniegelenk, was den Patienten an der Ausübung sportlicher Tätigkeiten hindert. Langfristig führt ein instabiles Kniegelenk auch zu einer Fehlbelastung von Knorpel und Meniskus, wodurch diese Strukturen geschädigt werden können.
Vorderes Kreuzband (VKB)
Ein gerissenes vorderes Kreuzband heilt meist nicht wieder zusammen, sodass bei aktiven Patienten in der Regel ein Ersatz dieses Bandes empfohlen wird. Zum Ersatz des vorderen Kreuzbandes werden in unserer Abteilung Kniebeugesehnen (die Sehnen des Musculus semitendinosus und Musculus gracilis) bevorzugt verwendet (Abb. 2), welche über Bohrkanäle im Ober- und Unterschenkel ins Kniegelenk eingezogen werden (Abb. 3).

Abb. 2: Zum Ersatz des vorderen Kreuzbandes vorbereitete Sehnentransplantate (körpereigene Kniebeugesehnen).

Abb. 3: Linkes Bild: Intaktes vorderes Kreuzband; Mittleres Bild: gerissenes vorderes Kreuzband; Rechtes Bild: Mit körpereigenen Kniebeugesehnen ersetztes vorderes Kreuzband.
Hinteres Kreuzband (HKB)
Ein Riss des hinteren Kreuzbandes kann frühzeitig oft ohne Operation behandelt werden. Durch spezielle Schienen, die mindestens 12 Wochen getragen werden, wird versucht, die Bandenden zusammenzuführen, sodass sie wieder zusammenwachsen können. Bei länger zurückliegenden Rissen oder unzureichender Stabilität nach Schienenbehandlung wird das Band ähnlich wie beim vorderen Kreuzband durch körpereigene Sehnen arthroskopisch ersetzt.

Abb. 4: Linkes Bild: Intaktes hinteres Kreuzband; Rechtes Bild: Mit körpereigenen Kniebeugesehnen ersetztes hinteres Kreuzband.
Seitenbänder
- Innenband: Häufig ist keine Operation notwendig; meist heilt der Riss durch das Tragen einer Schiene für 6 Wochen aus.
- Außenband: Muss dagegen häufig operiert werden. Je nach Lokalisation und Schweregrad des Risses wird das Band genäht, über kleine Knochenanker am Ober- bzw. Unterschenkel fixiert oder mit einer körpereigenen Sehne ersetzt.
Komplexe Bandverletzungen

Mit einer körpereigenen Sehne ersetztes Außenband.

Meniskusverletzungen: Ursachen und Behandlung
Funktion der Menisken:
Die beiden Menisken (Innen- und Außenmeniskus) übernehmen eine wichtige Funktion bei der Lastübertragung des Kniegelenkes. Kommt es zu einem Verlust von Meniskusgewebe, erhöht sich der Druck auf den Knorpel, wodurch dieser langfristig geschädigt wird und sich eine Arthrose (Gelenkverschleiß) bilden kann. Meniskusrisse machen sich in der Regel durch Schmerzen bei Belastung (z.B. Drehbewegungen) bemerkbar.
Behandlungsmöglichkeiten
- Meniskusnaht: Bei geeigneten Rissen, insbesondere im gut durchbluteten Bereich des Meniskus, wird eine Naht durchgeführt, um das Gewebe zu erhalten.

- Teilresektion: Wenn eine Naht nicht möglich ist, werden nur die beschädigten Teile des Meniskus entfernt, um so viel funktionelles Gewebe wie möglich zu erhalten.
Meniskusersatz
Musste in einer vorangegangenen Operation ein Großteil des Meniskus entfernt werden, kann in bestimmten Fällen zum langfristigen Schutz des Gelenkknorpels insbesondere bei jungen Patienten die Implantation eines Ersatzmeniskus erwogen werden.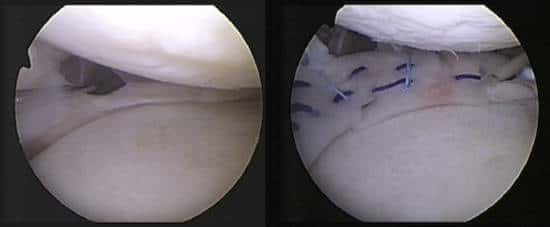
Linkes Bild: Nur noch im Randbereich vorhandener Meniskus; Rechtes Bild: Kniegelenk nach Implantation eines Ersatzmeniskus aus Kollagen.
Individuelle Beratung & modernste Behandlungsmethoden
Minimal-invasive & innovative OP-Techniken
Schnelle Rückkehr in Alltag, Beruf & Sport
Knorpelschäden: Ursachen und Behandlung
Ursachen
Behandlungsmöglichkeiten
- Mikrofrakturierung: Anbohren des Knochens unter dem Knorpelschaden, um die Bildung von Ersatzknorpel zu fördern.
- Knorpeltransplantation: Transplantation von körpereigenem Knorpelgewebe in den geschädigten Bereich.
- Knorpel-Knochen-Zylinder-Transplantation (OATS): Übertragung von Knorpel-Knochen-Zylindern aus weniger belasteten Bereichen in den Defekt.

Arthrose (Gelenkverschleiß): Ursachen und Behandlung
Ursachen
Behandlungsmöglichkeiten
- Konservativ: Physiotherapie, Schmerzmedikation und Injektionen.
- Operativ: Bei fortgeschrittener Arthrose kann ein Gelenkersatz (Endoprothese) notwendig sein, um die Funktion und Lebensqualität zu verbessern.

Abb. 9: Belastung des Kniegelenkes bei einem O-Bein. Die rote Linie beschreibt die Belastungsachse, welche vom Hüftkopf zum Sprunggelenk verläuft. Diese schneidet das Kniegelenk bei einem O-Bein im inneren Anteil des Kniegelenkes.
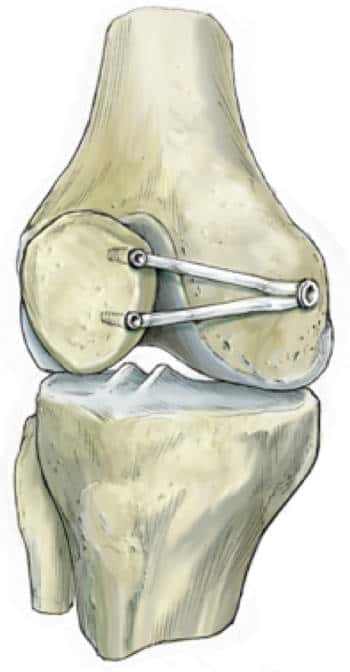
Fehlstellungen der Beine und Umstellungsoperationen
Bei einem O-Bein verläuft die Belastungsachse durch den inneren Anteil des Kniegelenkes (Abb. 9). Auf Dauer kann dies zu einer Überlastung mit Schmerzen und zu einem Knorpelverschleiß (Arthrose) führen. Bei einem X-Bein kommt es entsprechend zu einer Überlastung des äußeren Anteils des Kniegelenkes.
Umstellungsoperation
Bei Fehlstellungen kann eine sog. Umstellungsoperation durchgeführt werden. Hierbei wird über einen Sägeschnitt im Knochen die Ausrichtung des Beins korrigiert, sodass der beschädigte Anteil des Gelenks entlastet wird.

Linkes Bild: Die rote Linie zeigt die Belastungsachse vor dem Sägeschnitt. Diese verläuft durch den inneren Anteil des Kniegelenks; Rechtes Bild: Die grüne Linie zeigt die Belastungsachse nach dem Sägeschnitt und anschließender Korrektur der Beinachse. Die Belastung verläuft nun deutlich weiter außen, sodass der geschädigte innere Anteil des Gelenkes entlastet wird.
Je nachdem ob die Fehlstellung im Ober- oder Unterschenkel ihren Ursprung hat, wird der Sägeschnitt auch entsprechend am Unter- oder Oberschenkel durchgeführt. Bei einem O-Bein erfolgt die Korrektur meist am Unterschenkel, bei einem X-Bein meist am Oberschenkel.
Nach der Korrektur muss der Knochen wie bei einem Knochenbruch zunächst über eine Platte stabilisiert werden, welche nach ca. einem Jahr wieder entfernt werden kann.

Röntgenbild nach einer Umstellungsoperation am Unterschenkel bei einem O-Bein. Der Sägeschnitt wurde durch eine Platte aus einem Carboncompound-Material stabilisiert.
Verletzungen der Kniescheibe
Patellaluxation und operative Stabilisierung
Nach einer Ausrenkung der Kniescheibe (sog. Patellaluxation) kommt es meist zu einer Instabilität der Kniescheibe, wobei diese immer wieder „herausspringt“. Neben einer deutlichen Einschränkung für den Patienten beim Sport oder im Alltag kommt es zu einer zunehmenden Schädigung des Knorpels. Insbesondere bei jüngeren Patienten wird daher eine operative Stabilisierung der Kniescheibe empfohlen. Die häufigste Operationsmethode ist hierbei der Ersatz des Haltebandes der Kniescheibe (sog. mediales patellofemorales Ligament) mit einer körpereigenen Sehne (Sehne des Musculus Gracilis)(Abb. 12).
Risikofaktoren für Kniescheibeninstabilität
Behandlung von Knorpelschäden der Kniescheibe
Knorpelschäden der Kniescheibe werden identisch zu anderen Knorpelschäden behandelt. Nähere Informationen zur Behandlung von Knorpelschäden.
Mini-Prothese für fortgeschrittene Arthrose
Über besondere Erfahrung verfügt unsere Abteilung beim Teilersatz des Kniescheiben-Gelenks. Dies wird dann notwendig, wenn bereits ein fortgeschrittener Verschleiß des Gelenkknorpels vorliegt und biologische Verfahren, wie z. B. eine Knorpelzelltransplantation, nicht mehr möglich sind. In diesem Fall wird der geschädigte Bereich durch eine spezielle Mini-Prothese, welche von unserer Abteilung mitentwickelt wurde, ersetzt.

Röntgenaufnahmen nach einem Teilersatz des Kniescheibengelenkes mit einer Mini-Prothese.
Jetzt Termin vereinbaren!
Sie leiden unter Knieschmerzen oder einer Verletzung? Unsere Spezialisten der Sportorthopädie München bieten Ihnen modernste Diagnostik und maßgeschneiderte Therapien.
Lassen Sie sich beraten!
Vereinbaren Sie jetzt einen Termin zur persönlichen Untersuchung und Behandlung:
+49-(0)89 4140-7840
sportortho@mri.tum.de
Haus 524
Ismaninger Str. 22
81675 München

